Exploring the Link Between Trauma, PTSD, and Eating Disorders: A Comprehensive Study
Traditionally, the consensus in the eating disorder (ED) field had been to avoid trauma work during intensive treatment, opting to address it later in outpatient settings. This approach may arise from concerns about exacerbating eating disorder symptoms or a lack of expertise in trauma assessment and treatment.
However, recent research published in the Journal of Eating Disorders suggests that concurrent, parallel, and interwoven treatment for both the eating disorder and PTSD can be effectively delivered by the same providers/therapists during the same treatment course at the residential level of care.
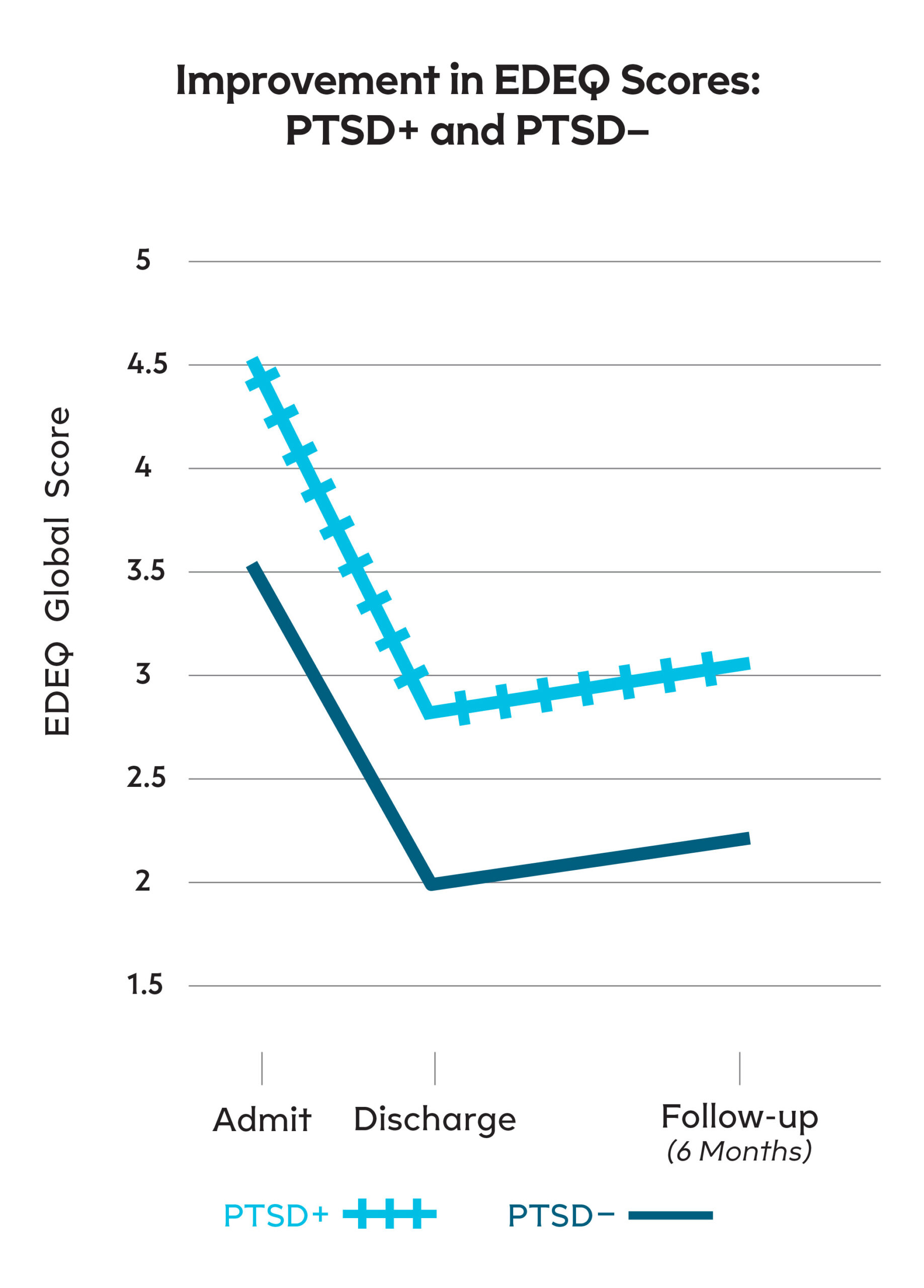
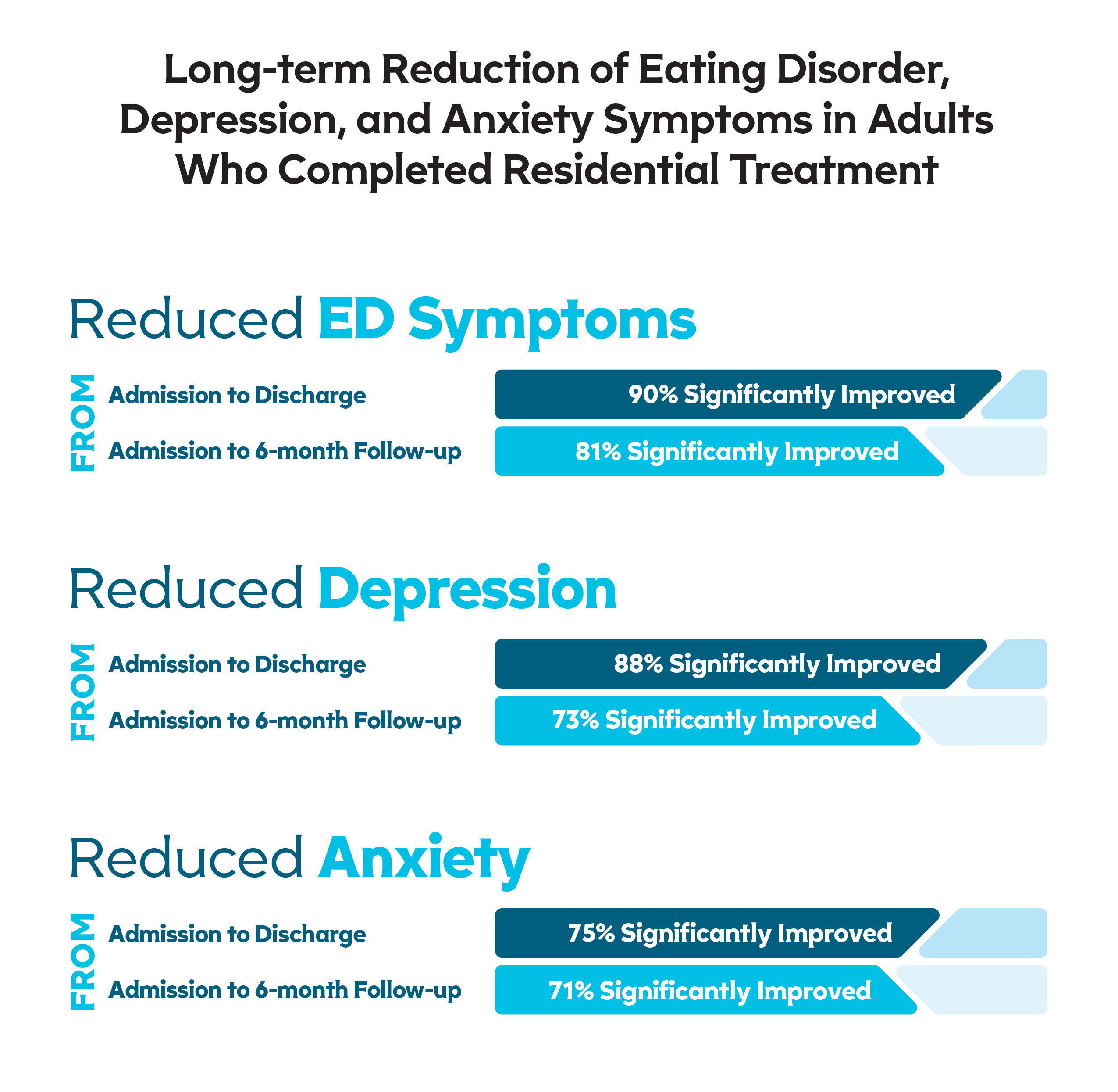
Integrated treatment strategies addressing PTSD for clients with eating disorders in residential settings have demonstrated lasting improvements six months post-discharge. These findings offer optimism that the eating disorder field can develop and implement tailored and concurrent approaches for individuals with PTSD undergoing higher levels of care for eating disorder treatment.
A Groundbreaking Study on PTSD and Eating Disorders
A recent study, conducted across seven residential treatment sites in the U.S., has unveiled significant insights into the relationship between traumatic experiences, post-traumatic stress disorder (PTSD), and the severity of eating disorder symptoms. The study, involving 609 adult participants (96% female) who received residential treatment for an eating disorder, utilized validated self-report measures to gauge the extent of ED symptoms, PTSD, major depression, state-trait anxiety, and overall quality of life.
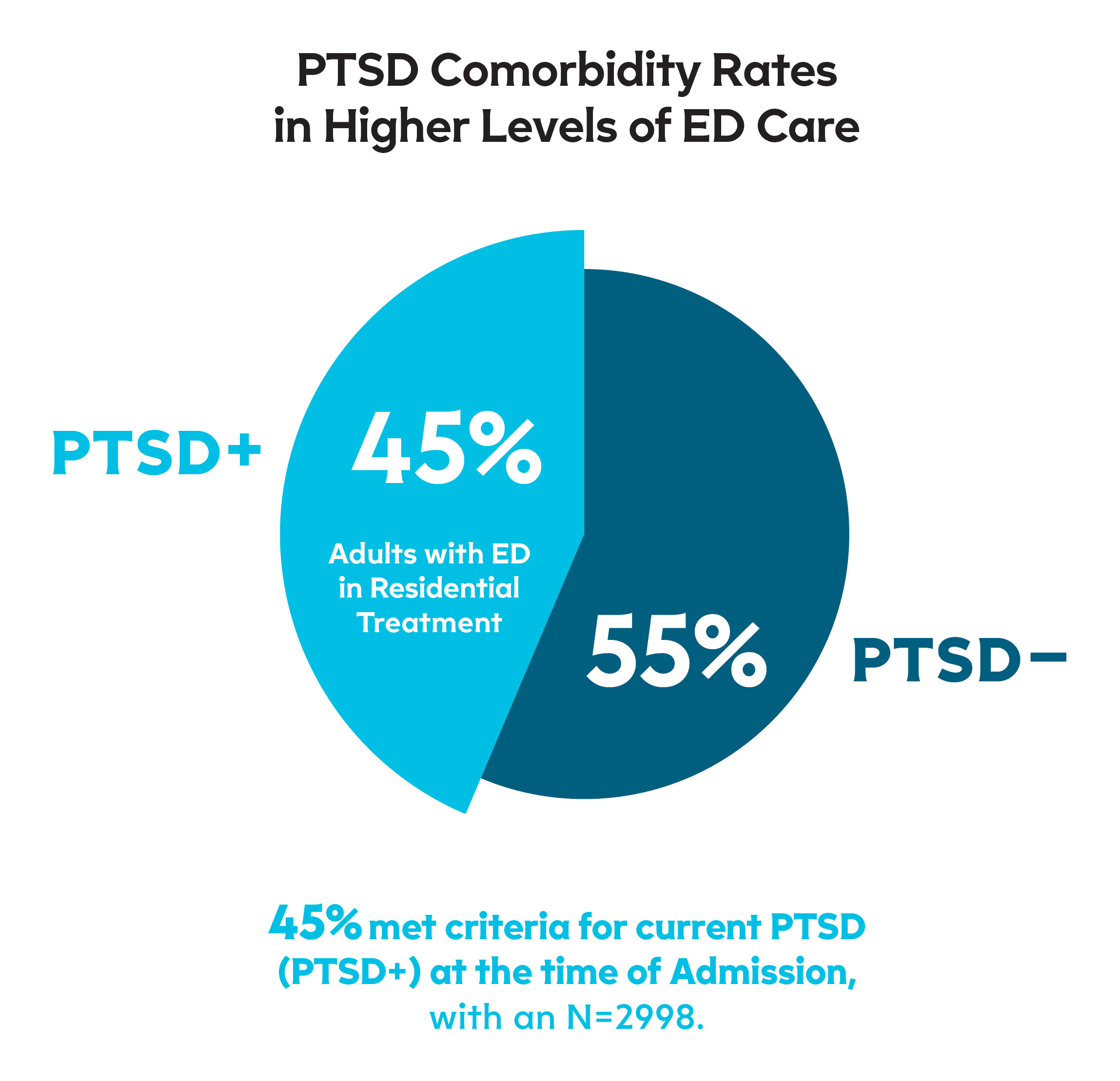
High Prevalence of PTSD in Eating Disorder Patients
One of the striking findings of this study is the prevalence of PTSD in the residential eating disorder treatment setting. Nearly half (49.3%) of the clients admitted for ED treatment exhibited symptoms compatible with PTSD, highlighting how common these comorbid conditions are in this demographic.
Trauma and Its Impact on Eating Disorders
The study found that patients with both ED and PTSD (ED-PTSD+) experienced a significantly higher number of traumatic life events compared to ED clients without PTSD. This group also showed higher rates of almost all types of lifetime traumatic events, particularly those associated with greater trauma exposure, such as sexual and physical assaults. These findings underline the critical role of trauma exposure in the development and maintenance of eating disorders, particularly those with binge-purge features.
Severity of Symptoms and Quality of Life
Clients with both an eating disorder and PTSD had notably more severe symptoms across all measures. These included symptoms of eating disorder pathology, as well as depression, state-trait anxiety, and a notably diminished quality of life. These findings suggest that the impact of PTSD on these individuals extends far beyond the eating disorder and to overall mental health and day-to-day functioning.
Implications for Treatment and Care
The findings from this study emphasize the need for integrated treatment approaches that effectively address the complex interplay between ED and PTSD. This research adds to the growing body of evidence suggesting that patients with co-occurring ED and PTSD have more complex clinical presentations that would benefit from specialized, trauma-informed care strategies. The study’s outcomes pose significant opportunities for ED treatment programs and practitioners, urging them to adopt more comprehensive, trauma-focused treatment protocols.
In summary, this study sheds light on the intricate relationships between trauma, PTSD, and eating disorders, highlighting the need for a nuanced approach to treatment that addresses both the psychological trauma and the symptoms of the eating disorder. The high prevalence of PTSD among individuals with eating disorders underscores the importance of considering trauma in the assessment and treatment of these complex conditions.
How does Monte Nido & Affiliates Treat Trauma?
At Monte Nido & Affiliates, we go beyond trauma-informed care by being the first to provide evidence-based trauma treatments concurrently with ED treatment at higher levels of care. We integrate cognitive processing therapy (CPT), one of the three gold standard trauma treatments, in tandem with eating disorder treatment that complements cognitive behavioral therapy (CBT) and dialectical behavior therapy (DBT). 81% of patients with PTSD at admission had reductions in trauma symptom scores from admission to discharge and 73% from admission to follow-up (6 months later).
 “We support clients recovering from eating disorders by enhancing motivation and insight, developing healthy coping strategies, repairing and growing relationships, and changing the way clients understand themselves in their world,” said Molly Perlman, MD, MPH, CEDS, Chief Medical Director of Monte Nido & Affiliates. “Our comprehensive system of care ensures we treat clients with a multidimensional approach and includes relational focus, trusted outcomes, cultural awareness and building resilience through a trauma-informed approach.”
“We support clients recovering from eating disorders by enhancing motivation and insight, developing healthy coping strategies, repairing and growing relationships, and changing the way clients understand themselves in their world,” said Molly Perlman, MD, MPH, CEDS, Chief Medical Director of Monte Nido & Affiliates. “Our comprehensive system of care ensures we treat clients with a multidimensional approach and includes relational focus, trusted outcomes, cultural awareness and building resilience through a trauma-informed approach.”
If you’re interested in learning more about our programs, please visit www.MonteNidoAffiliates.com or email Admissions@MonteNidoAffiliates.com to connect with a member of our Admissions Team.
Monte Nido & Affiliates delivers clinically comprehensive, research-backed treatment to adults and adolescents with eating and co-occurring disorders, within a healing environment. As a Miami, FL-based company, Monte Nido & Affiliates has over 50 programs, offering a full continuum of care. Founded in 1996, Monte Nido & Affiliates specializes in the treatment of eating disorders for all genders and includes four distinct clinical programs: Monte Nido, Walden Behavioral Care, Clementine, and Rosewood Centers. For over two decades, our tenured and expert staff — which includes recovered professionals — has delivered treatment that leads to full recovery. For more information, please visit: montenidoaffiliates.com.